Immunology: Meaning, Types, Examples, Treatment, Symptoms
Immunology is the branch of medicine that studies immunity. It explains how the immune system works.Immunity is structure and functioning of the immune system. Its mechanisms to defend harmful pathogens. It protects the body from diseases. Immunology helps understand immune responses.Immunology helps us understand human health and disease.
This Story also Contains
- What is Immunology?
- What is the Immune System?
- Types of Immune System
- Table showing the Difference Between Innate Immunity and Adaptive Immunity
- How the Immune System Works
- Vaccines and Immunisation
- Symptoms of Immune Dysfunction
- Advances in Immunology
- MCQs on Immune System
The immune system detects foreign invades. It includes white blood cells and antibodies. Immunology explores vaccines and immunity. Autoimmune disorders are studied in immunology. Immunology helps develop effective treatments. Research in immunology improves human health. Immunology plays a big role in biology and medicine.
What is Immunology?
Immunology helps us understand how our bodies fight disease and resist it. The immune system protects against pathogens. It is key to modern healthcare. Immunology helps build strong immunity. Vaccination work based on immunology. Immunotherapy is a breakthrough treatment. Immunology supports disease prevention strategies.
The immune system has complex cells. It responds to foreign pathogens fast. Immunology explores autoimmune reactions too. Vaccines and CRISPR show new promise. Immunity research changes every year. Immunology helps control hypersensitivity issues. The future of immunology looks powerful.
What is the Immune System?
The immune system is a powerful defence network in the body. It functions to protect the body from infections, disease, and even tumour cells.This system includes specialized cells, tissues, and organs.The interaction between antigen and immunology is central to understanding how the immune system identifies and responds to harmful invaders. The immune system can recognize and eliminate pathogens while maintaining tolerance to self-components.
Immunity and immune system is the study of this complex defence system. It explains how the immune system recognizes threats and responds to them. Scientific studies uncover the hidden mechanisms of diseases, thereby opening doors to new treatments and interventions to deal with a wide range of health issues. Immunology helps in developing vaccines, immunotherapies, and treatments for autoimmune diseases.
Types of Immune System
There are two types of immune systems, which are classified based on whether they are present at the time of birth or not:
Innate Immune System.
Adaptive Immune System.
Innate Immunity
Innate immunity, the first level of defence against infectious agents and other foreign substances, is very fast in response and neutralizes potential threats quickly.
The first line of defence includes physical, chemical, and mechanical barriers: the skin, mucous membranes, enzymes, and antimicrobial proteins that actively prevent pathogen entrance.
White blood cells, such as macrophages and neutrophils, are important cellular components of the mechanisms. Innate immunity operates to engulf and subsequently destroy invading foreign substances, in a process called phagocytosis.
Innate immunity provides general protection without any need for prior exposure to or recognition of a pathogen.
Adaptive Immunity
Adaptive immunity is the second line of defence in the body.
This includes specific lymphocytes (B and T cells) with antibodies.
Adaptive immunity uniquely provides reactions towards pathogens.
Adaptive immunity provides immunological memory and, therefore, improvement in resistance to future encounters with the same pathogens.
T cells play central roles in cell-mediated immunity: helper T cells coordinate the immune responses, cytotoxic T cells kill the infected or otherwise damaged cells, and the regulatory T cells fine-tune the overall intensity of the immune response and maintain the immune tolerance.
Table showing the Difference Between Innate Immunity and Adaptive Immunity
The immune system has two major types of defence: innate immunity and adaptive immunity. Innate immunity acts as the first line of defence. Adaptive immunity is slower, but more targeted and long-lasting. Here's a table showing the key differences between innate immunity and adaptive immunity:
Innate Immunity | Adaptive Immunity |
The response is quick. | The response is slow. |
Not specific in nature. | Highly specific. |
Does not have memory related to immunology. | It has the memory associated with immunology. |
It gives an immediate protection to the body. | It gives long-term protection to the body. |
Key components of this immunity are physical barriers like skin. | Key components of this immunity are antibodies and B and T cells. |
Present from birth | Develops after exposure to germs |
How the Immune System Works
A well-organised and intricate sequence of events occurs in the immune system when pathogens are encountered. Such a response includes recognising them, mounting an effective reaction, and developing immune memory.
Recognition
The immune system contains specific receptors, known as pattern recognition receptors (PRRs). It allows for pathogen detection. They identify specific molecular patterns on their surface, known as pathogen-associated molecular patterns (PAMPs).
Macrophages, dendritic cells, and neutrophils also express PRRs. Furthermore, epithelial cells, along with other tissues, also have these receptors. When PRRs come into contact with pathogens, they trigger immune responses signalling cascades.
Response
When germs enter the body, the immune system reacts. Phagocytosis is one way the body fights back. Neutrophils and macrophages swallow and destroy the germs. Another way is by making antibodies.
B cells become plasma cells, which release antibodies. These antibodies attack germs or help other cells kill them. Some antibodies carry germs to lymph nodes for removal.
Memory
After infection, the body makes memory B and T cells. These cells help stop the same infection in the future. Memory B cells quickly make antibodies during reinfection. Memory T cells respond faster when the same germ comes back. This makes the second immune response quicker and stronger.
Similarly, upon re-encounter with specific antigens, the reactivity of memory T cells is improved, a development that aids in the quick elimination of pathogens and disease containment.
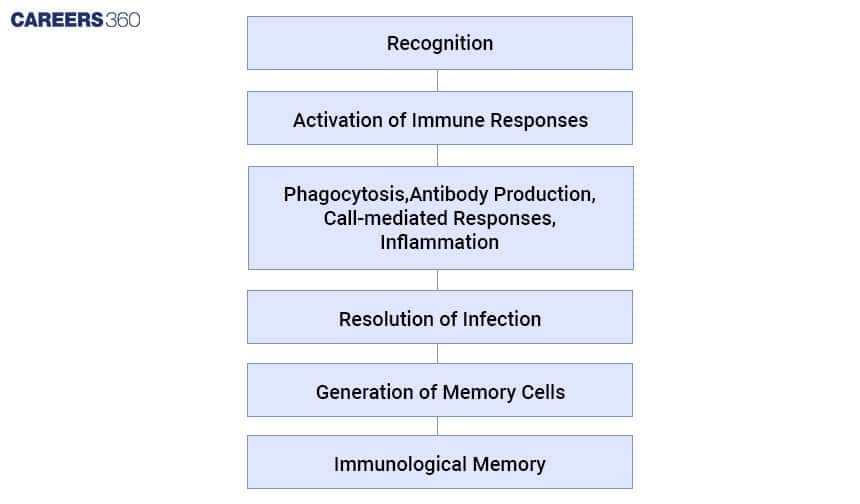
This flowchart displays the sequential steps implicated in the immune response process from the recognition of pathogens to the establishment of immunological memory, emphasising the main principles or constituents of the immune system’s defence mechanisms against infections.
Vaccines and Immunisation
Vaccines work by making our immune systems able to learn about or recognise particular pathogens without being the actual disease itself. Often, they contain very similar or dead versions of these harmful invaders, or bits and pieces of them called antigens. Once they are given, our bodies start producing things like antibodies and memory cells that are used as weapons against harmful organisms when we happen to get infected again, for instance.
Importance of Vaccination
To avoid the spread of diseases and decrease illness and death rates in human society. Smallpox has been killed by the use of such vaccines as vaccination while others like polio have been suppressed remarkably. Therefore, immunising against any disease means, one does not only protect him or herself from that particular ailment but also safeguards the less fortunate members. That is why people are supposed to be immunised fully.
Symptoms of Immune Dysfunction
Immune dysfunction happens when the immune system is overactive, underactive, or defective. It can lead to chronic infections, autoimmune disorders, or immunodeficiency syndromes. Below is a table showing some common conditions and their related symptoms.
CONDITION | SYMPTOMS |
Autoimmune Diseases | Joint pain, fatigue, skin rashes, organ involvement |
Rheumatoid Arthritis | Joint pain, stiffness, swelling, fatigue |
Severe Combined Immunodeficiency (SCID) | Severe, recurrent infections, failure to thrive |
Chronic Granulomatous Disease (CGD) | Chronic Granulomatous Disease (CGD) |
HIV/AIDS | Fatigue, swollen lymph nodes, recurrent infections |
Advances in Immunology
New discoveries in immunology have helped treat many diseases. These advances make the immune system stronger and smarter. They help fight cancer and other serious conditions.
New Therapies: New cancer treatments use the immune system. Drugs like pembrolizumab and nivolumab help fight cancer. They help the immune system find and kill tumour cells. CAR-T cell therapy uses special T cells to kill blood cancer. These therapies give hope to many patients.
Immunotherapies for Cancer: Cancer patients use immunotherapy to boost the body's immune system by recognising and destroying tumour cells. Old methods include checkpoint drugs and CAR-T therapy. New methods include cancer vaccines and oncolytic viruses. These may help treat more types of cancer.
Role of CRISPR in Immune System Research:CRISPR is a gene-editing tool. It helps scientists study the immune system. CRISPR can change genes in immune cells. It helps find new treatments and targets. It makes immune research faster and better.
MCQs on Immune System
Question: In ‘T-lymphocytes’, the letter ‘T’ refers to
Thalamus
Tonsil
Thymus
Thyroid
Answer: The T-lymphocytes, named for the thymus, are very important in the cell-mediated immune system. These immature lymphocytes start in the bone marrow. They move through the bloodstream to be in the thymus where they mature into functional T-lymphocytes. Once in the thymus, they receive selection processes that verify their ability to react upon antigens properly and avoid reacting against themselves. For a good, strong immune response, this matured state should occur.
Hence the correct answer is Option 3) Thymus
Question: The type of immunity in which a person’s own body produces an immune response in terms of antibodies against some kind of infection or vaccination is said to be
Passive immunity
Humoral immunity
Innate immunity
Active immunity
Answer: The type of immunity in question is active immunity.
Characteristics of Active Immunity:
- It involves the body's production of antibodies and memory cells as a response to an infection or vaccine.
- It is typically long-lasting due to the immune system's ability to remember pathogens for future defense.
Active Immunity can be initiated by:
- Natural infection: Exposure to a live pathogen (virus or bacterium) prompts the immune system to create a specific response.
- Vaccination: Introduction of a weakened or killed pathogen, or its components (e.g., proteins), which induces the creation of antibodies and memory cells without causing illness.
Hence, the correct answer is option 4) Active immunity.
Also Read:
Frequently Asked Questions (FAQs)
By activating the immune system within the human body against cancer, autoimmune diseases, etc., immunotherapy contributes significantly to the medical revolution. It makes use of immune checkpoint inhibitors, CAR-T cell therapy, and monoclonal antibodies.
Specific receptors known as pattern recognition receptors (PRRs) help to identify pathogen-associated molecular patterns (PAMPs) on the surface of pathogens. This is a process by which the human immune system can recognise disease-causing organisms. Immune responses are elicited once a pathogen has been discovered by PRRs located on some immune cells, such as macrophages and dendritic cells, or even on epithelial cells themselves.
Some common techniques used in research and diagnostics concerning the detection of antibodies or antigens are:
Enzyme-linked immunosorbent assays (ELISAs)
Flow cytometry can be used to analyse populations of cells or their functions.
CRISPR-Cas9 allows us to edit genomes by changing genes around using RNA that is transported into cells with the help of bacterial proteins called Cas9, either to add new genes or switch others off at will.
Adaptive immunity is much more specific than innate immunity because it produces memory cells to guard against particular pathogens in the long run. Meanwhile, innate immunity operates instantly with non-specific methods such as inflammation or phagocytosis.
Conditions, like rheumatoid arthritis and lupus, present with joint pain, fatigue, skin rashes and organ involvement, as shown by symptoms of autoimmune diseases.
